The long-awaited solution to replace narcotic pain medications
Discover Taphalgin, the revolutionary, non-narcotic analgesic changing the face of pain management. Taphalgin effectively targets acute and chronic pain, offering a safer and more convenient alternative to common narcotic-analgesics. It's not just an analgesic; it's a new era of pain relief – self-administered, with minimal side effects, no accumulation in the body, and no tolerance development upon repeated use.

First in class, non-narcotic peptide analgesic with a dual mechanism of action

No Tolerance Development

No Accumulation

Patient-Friendly Pain Solution
About Taphalgin
Taphalgin is an innovative analgesic that offers a valuable alternative to widely used narcotic drugs like morphine. It provides efficient pain management without the risks associated with narcotics. Non-habit-forming and with minimal side effects, Taphalgin has undergone successful phase 3 clinical trials, demonstrating its potent pain-relieving capabilities across various therapeutic applications.
As a prescription-only medication, Taphalgin offers healthcare professionals a powerful tool for enhancing patient care and improving quality of life. Its innovative approach to pain relief represents a significant step forward, providing a safer and more effective option for patients.
What sets Taphalgin apart is its ability to deliver comprehensive pain relief while maintaining consciousness and functionality. Patients experience complete pain elimination, remaining fully aware and able to perform daily activities.
Taphalgin is particularly effective in managing pain in patients with cancer and other malignant diseases. It addresses both acute and chronic pain, whether during and after treatments or in advanced stages of the disease. It also plays a vital role in trauma and post-surgical pain management.
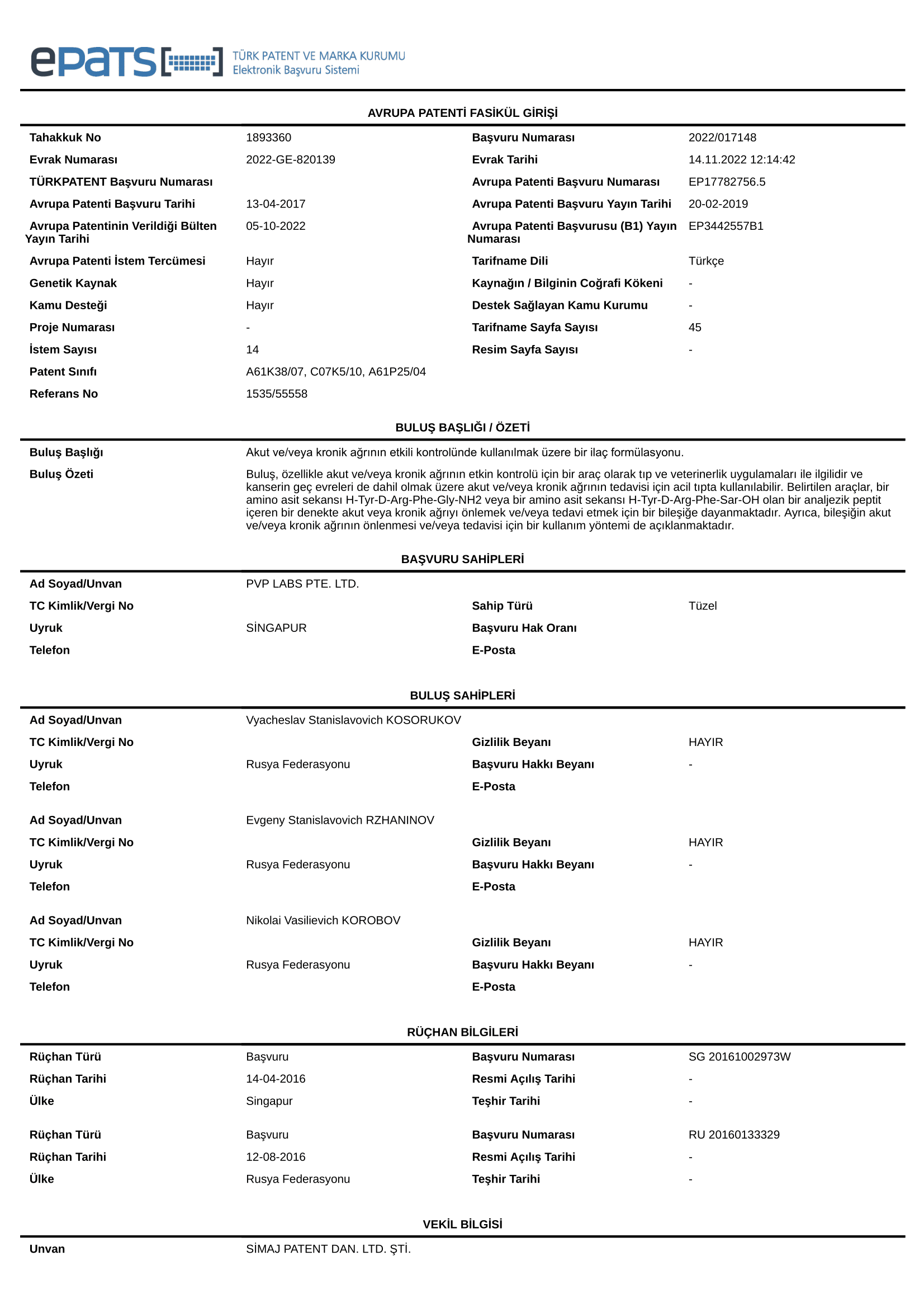
Mechanism of Action
Taphalgin (L-Tyrosyl-D-arginyl-L-phenylalanylglycinamide) is a highly selective agonist of MOR1 (μ1-opioid receptor) and exerts little to no impact on other opioid receptors (MOR2, MOR3, KOR, DOR). Interaction with δ-receptors is three orders of magnitude weaker than with μ-receptors.
Taphalgin interacts with both peripheral and central receptors, primarily acting at the spinal level.
High selectivity to μ1-opioid receptor ensures the absence of side effects typical of most opioid narcotic medications. It is worth clarifying that the activation of μ2-opioid receptors can result in side effects such as respiratory depression, cardiovascular system disturbances and suppression of intestinal mobility.
Taphalgin also possesses a secondary antinociceptive mechanism of action realized through the inhibition of calcium channels. Once Taphalgin binds to μ1-receptors, the G protein complex is released, inhibiting the release of neurotransmitters.
Its high selectivity to μ1-opioid receptors and its calcium channel-mediated antinociceptive activity are responsible for the substance's highly specific activity and its low abuse potential, even following multiple doses or overdoses.
Taphalgin activates the anti-nociceptive system and disrupts interneural transmission of pain signals at different CNS levels and alters pain perception intensity.
As a peptide, Taphalgin does not accumulate in the body and participates in the natural receptor desensitization and recovery following activation without disturbing this process, ensuring that tolerance to the antinociceptive activity does not develop after multiple doses.
Possible therapeutical areas
Conditions for treatment with Taphalgin
Taphalgin, like morphine, Promedol, and other opioid analgesics, is used as an analgesic for patients with injuries and various diseases that are associated with severe pain.
Taphalgin, like morphine, Promedol, and other opioid analgesics, is used as an analgesic for patients with injuries and various diseases that are associated with severe pain.
Oncology Application
Pain is highly prevalent in the cancer population. Virtually all patients with malignant disease experience recurrent episodes of acute pain, which may accompany surgery, invasive procedures, or complications. While pain can occur at any stage of the disease, it typically increases in frequency and intensity as the cancer progresses. It has been reported that approximately 40% of cancer patients suffer pain after curative treatment, 55% during cancer treatment, and 66% in advanced stages of the disease—with one-third of patients describing pain levels as distressing or intolerable.

Postoperative Pain
Postoperative pain is an anticipated and temporary (up to several days) increase in background pain that occurs after a surgery. Pain at the surgery site is especially intensive in the first few days after surgery and, if remained untreated, it can delay the patient's recovery. That is why pain relief after surgery remains one of the major medical challenges. During a clinical trial in patients with surgical interventions Taphalgin, solution for subcutaneous administration, was as effective as Promedol, solution for injection.

Burns
According to many experts, morphine is the drug of choice for burn management. In the case of Taphalgin administration, relief of thermally induced pain was conclusively demonstrated in animals.

Cardiology
Taphalgin can be used in myocardial infarction or unstable angina — i.e. conditions associated with severe pain. The need for such analgesic treatment arises quite often, as cardiac diseases are some of the most common morbidities.
Additional possible indications for Taphalgin

Childbirth
At present, analgesia during labour is provided by epidural anaesthesia, but it has its own adverse side effects, such as loss of leg mobility, urination problems, etc. The use of Taphalgin during labour and delivery is potentially beneficial, because unlike morphine, Taphalgin does not cause respiratory depression in the mother or foetus and does not suppress smooth muscle activity, which could otherwise interfere with labour.
Neuropathic pain
A marked reduction of migraine headaches was observed in isolated cases when the product was used at dosages as small as 0.1 of the therapeutic doses. The effect of the drug is significantly enhanced by its ability to suppress N-calcium channels, which can help reduce neuropathic pain. Possible uses include neuropathic pain treatment in the form of a transdermal patch.

Addiction treatment
Based on the mechanism of action, Taphalgin has a potential of treating drug addiction at the abstinence stage.
Dosing

Final dosage form
Solution for subcutaneous administration.
Mode of administration
Subcutaneously (s/c). Solution for subcutaneous administration - in pre-filled syringes or vials.
Dosing
The dose is selected individually for each patient, taking into account the pain severity and individual sensitivity to the drug. The recommended starting doses are 2 mg 3 times per day or 4 mg 2 times per day, if necessary, a single dose can be increased in increments of 1-2 mg to 7 mg, or reduced if adequate analgesia is maintained.
Subcutaneous administration
Subcutaneous administration The subcutaneous route of administration is quite convenient for the patient, can be performed independently by the patient or a caregiver. The volume of the injected drug is small and the injection is comfortably tolerated by patients.